Neurological signs are obviously not an outcome of SARS-CoV-2 infection of the brain.
Researchers still are uncertain how neurological signs develop in COVID-19 Is it due to the fact that SARS-CoV-2 contaminates the brain? Or are these signs the outcome of swelling in the remainder of the body? A research study by Charité– Universitätsmedizin Berlin has actually now produced proof to support the latter theory. It was released today in the journal Nature Neuroscience
Headaches, memory issues, and tiredness are simply a few of the neurological effects that develop throughout coronavirus infection and can last well beyond the intense duration. Even early on in the pandemic, scientists speculated that direct infection of the brain might be the cause.
” We took that as our hypothesis at the start, too. However up until now, there has actually been no clear proof that the coronavirus can continue the brain, not to mention multiply,” describes Dr. Helena Radbruch, head of the Persistent Neuroinflammation working group at the Department of Neuropathology at Charité. “For that, we would require to discover proof of undamaged infection particles in the brain, for instance. Rather, the signs that the coronavirus might contaminate the brain originated from indirect screening approaches, so they aren’t totally definitive.”
According to a 2nd hypothesis, the neurological signs would rather be a type of negative effects of the strong immune reaction the body releases to resist the infection. Previous research studies have actually produced signs that this may be the case. The present Charité research study now strengthens this theory with comprehensive molecular biology and physiological arise from autopsies.
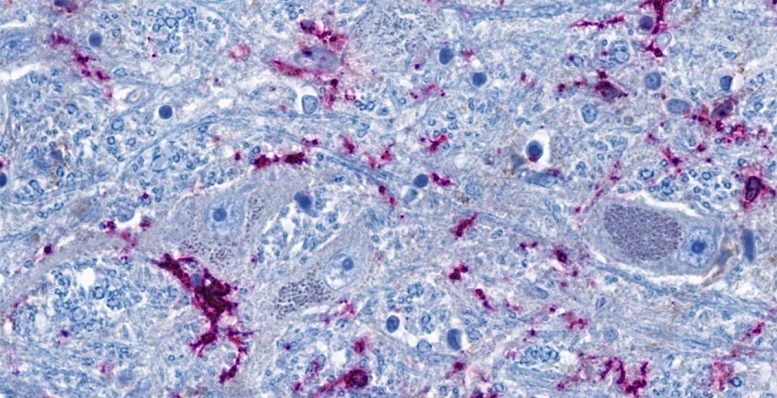
Cross-section of the brainstem: Nerve cells (blue-gray) remain in close contact with immune cells (purple). The threadlike blue structures are extensions of the nerve cells, which can reach all the method into remote organs in the kind of nerve fibers. According to the research study, the immune cells and nerve cells in the brainstem can be triggered straight through the nerve fibers as an outcome of swelling in the lungs. Credit: © Charité|Jenny Meinhardt
No Indications of Direct Infection of the Brain
For the research study, the group of scientists examined different locations of the brain in 21 individuals who passed away in medical facility settings, usually in an ICU, due to extreme coronavirus infection. For contrast, the scientists studied 9 clients who passed away of other causes after treatment in extensive care. Initially, they aimed to see whether the tissue revealed any noticeable modifications and looked for any indicator of coronavirus. Then they performed an in-depth analysis of genes and proteins to determine the particular procedures that had actually happened inside private cells.
Like other groups of scientists before them, the Charité researchers discovered coronavirus hereditary product in the brain sometimes. “However we didn’t discover nerve cells contaminated with SARS-CoV-2,” Radbruch notes. “We presume that immune cells soaked up the infection in the body and after that took a trip to the brain. They’re still bring the infection, however it does not contaminate cells of the brain. So coronavirus has actually gotten into other cells in the body, however not the brain itself.”
Brain Responds to Swelling in the Body
Still, the scientists did note striking modifications in molecular procedures in some cells of the brain in those contaminated with COVID-19: For instance, the cells increase the interferon signaling path, which is usually triggered in the course of a viral infection.
” Some nerve cells obviously respond to the swelling in the remainder of the body,” states Prof. Christian Conrad, head of the Intelligent Imaging working group at the Berlin Institute of Health at Charité (BIH) and among the primary private investigators in the research study, in addition to Radbruch. “This molecular response might be an excellent description for the neurological signs we see in COVID-19 clients. For instance, neurotransmitters produced by these cells in the brainstem might trigger tiredness. That’s due to the fact that the brainstem is home to groups of cells that manage drive, inspiration, and state of mind.”
The reactive afferent neuron were discovered mostly in what are referred to as the nuclei of the vagus nerve. These are afferent neuron found in the brainstem that extend all the method to organs such as the lungs, intestinal tract, and heart. “In streamlined terms, our analysis of our information is that the vagus nerve ‘senses’ the inflammatory reaction in various organs of the body and responds to it in the brainstem– without there being any real infection of brain tissue,” Radbruch describes. “Through this system, the swelling does spread out from the body to the brain in such a way, which can interfere with brain function.”
Limited-Time Response
The nerve cells’ response to the swelling is momentary, as revealed by a contrast of individuals who passed away throughout an intense coronavirus infection with those who passed away a minimum of 2 weeks later. The molecular modifications are most obvious throughout the intense infection stage, however they do stabilize once again later– a minimum of in the huge bulk of cases.
” We believe it’s possible that if the swelling ends up being persistent, that might be what triggers the neurological signs typically observed in long COVID in some individuals,” Conrad states. To act on this suspicion, the group of scientists is now preparing to study the molecular signatures in the cerebral fluid of long COVID clients in higher information.
Referral: “Proteomic and transcriptomic profiling of brainstem, cerebellum and olfactory tissues in early- and late-phase COVID-19” by Josefine Radke, Jenny Meinhardt, Tom Aschman, Robert Lorenz Chua, Vadim Farztdinov, Sören Lukassen, Foo Wei 10, Ekaterina Friebel, Naveed Ishaque, Jonas Franz, Valerie Helena Huhle, Ronja Mothes, Kristin Peters, Carolina Thomas, Shirin Schneeberger, Elisa Schumann, Leona Kawelke, Julia Jünger, Viktor Horst, Simon Streit, Regina von Manitius, Péter Körtvélyessy, Stefan Vielhaber, Dirk Reinhold, Anja E. Hauser, Anja Osterloh, Philipp Enghard, Jana Ihlow, Sefer Elezkurtaj, David Horst, Florian Kurth, Marcel A. Müller, Nils C. Gassen, Julia Melchert, Katharina Jechow, Bernd Timmermann, Camila Fernandez-Zapata, Chotima Böttcher, Werner Stenzel, Elke Krüger, Markus Landthaler, Emanuel Wyler, Victor Corman, Christine Stadelmann, Markus Ralser, Roland Eils, Frank L. Heppner, Michael Mülleder, Christian Conrad and Helena Radbruch, 16 February 2024, Nature Neuroscience
DOI: 10.1038/ s41593-024-01573-y